General Public's Knowledge, Attitude and Practice Survey on Antibiotic Resistance 2023
Release date: 20 November 2024
General Public's Knowledge, Attitude and Practice Survey on Antibiotic Resistance 2023
Introduction
The Centre for Health Protection (CHP) conducts regular surveys to monitor the trend of general public’s knowledge, attitude and practice on antibiotic resistance and to assess the effectiveness of public health interventions. The Survey on General Public’s Knowledge, Attitude and Practice on Antibiotic Resistance 2023 (KAP Survey) was commissioned to the Telephone Survey Research Laboratory of Hong Kong Institute of Asia-Pacific Studies of The Chinese University of Hong Kong.
Survey Method
The KAP Survey adopted the same method as the last round of survey in 2022. The target population consisted of non-institutional Hong Kong residents aged 15 or above who could speak Cantonese, Putonghua or English (excluding foreign domestic helpers). The survey was conducted from 27 November 2023 to 8 January 2024 through landline and mobile telephone interviews via random sampling. A sample size of 1,083 successful interviews (426 through landline numbers and 657 from mobile numbers) was achieved, with an overall response rate of 50.1%.
The key findings of the KAP Survey included:
- Knowledge and Awareness
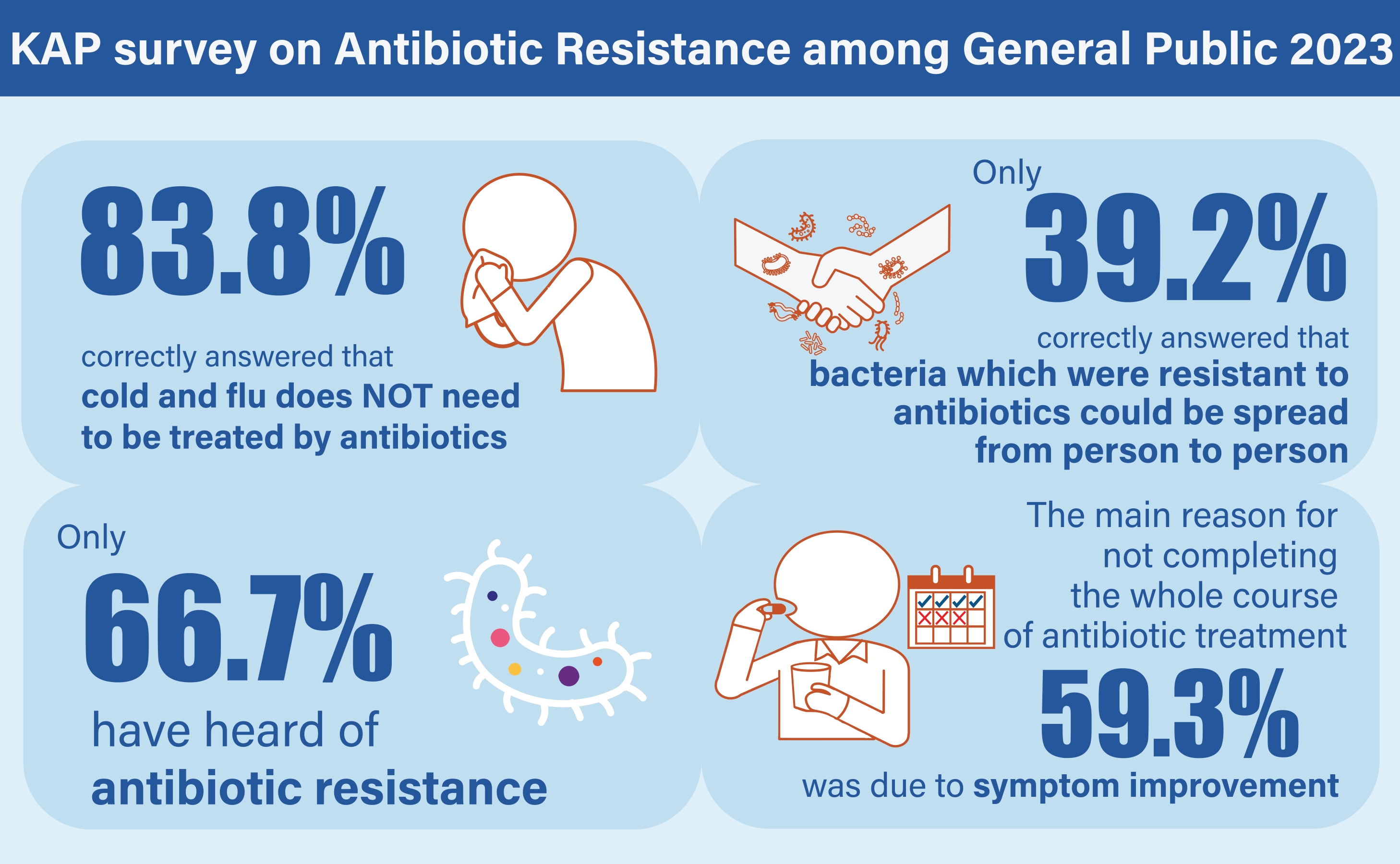
- More than half of all respondents have heard of the terms “drug-resistant bacteria” (66.6%) and “antibiotic resistance” (66.7%) in either Chinese or English.
- The majority of the respondents (83.8%) correctly answered that cold and flu does not need to be treated by antibiotics.
- Less than half of the respondents (39.2%) correctly answered that bacteria which were resistant to antibiotics could be spread from person to person.
- Among those whose last course of antibiotics was prescribed by doctors, only 19.7% reported that they had noticed the health advice (e.g. disinfect and cover all wounds) on the antibiotic medicine bag.
- In terms of awareness of food safety, only 71.4% of respondents correctly understood that thorough cooking is effective in killing drug-resistant bacteria in food. About three-quarters (73.7%) of the respondents correctly understood that if high-risk individuals (including pregnant women, young children, the elderly and people with weakened immune systems) avoid consuming raw or undercooked ready-to-eat food, their risk of being infected by drug-resistant bacteria from food will be reduced.
- Attitude
- When a doctor’s initial assessment indicated that antibiotics are not needed, the vast majority of respondents (94.7%) would accept the doctor’s advice to observe for a few more days or to wait for the diagnostic test result before deciding whether to prescribe antibiotics or not.
- Less than half of all respondents (49.5%) wanted their doctor to share decision-making on antibiotics prescription with them.
- Practice
- Among respondents who had ever taken antibiotics, the vast majority (97.1%) reported that their last taken antibiotics were prescribed by doctors.
- Among respondents (46.7% of all respondents) who reported that they had consulted a doctor (for cold or flu) in the past 12 months, only 3.6% requested antibiotics during that consultation.
- Among respondents whose last course of antibiotics was prescribed by a doctor, 7.1% did not complete the whole course of treatment as instructed, with the main reason (59.3%) being symptom improvement.
Observations and Recommendations
This Survey was conducted after the COVID-19 pandemic when normalcy and social activities had resumed. The proportion of respondents who had taken antibiotics in the preceding year increased from 26.1% in 2022 to 36.6% in 2023, revealing an increase in antimicrobial use after COVID-19. This finding could be due to the rebound of respiratory infections, as reflected in the increase in percentage of respondents having consulted doctors for cold/flu (from 21.6% in 2022 to 46.7% in 2023). Overall, this may reflect in both the appropriate use of antibiotics to treat bacterial infections and the inappropriate use for viral diseases.
There were decreases in the percentage of respondents who had heard of the terms “Antibiotic Resistance/抗生素耐藥性” (from 76.0% to 66.7%), and “Antimicrobial Resistance/抗菌素耐藥性” (from 40.3% to 22.6%). Moreover, a lower percentage of respondents knew that antibiotic-resistant bacteria could be spread from person to person (from 44.1% to 39.2%). In light of the knowledge deficit among the public, more intensive health education and promotion activities should be conducted to raise public knowledge and awareness of antimicrobial resistance through easy-to-understand and impactful media channels.
This survey also revealed that a significant proportion of respondents did not wish to share decision-making with doctors on antibiotics prescription (66.3% in 2022 and 49.5% in 2023). However, the majority would accept a doctor’s advice to observe when the initial assessment indicated that antibiotics were not needed. Given their continuity of care, primary care doctors are in the best position to minimise the spread of antibiotic resistance by practicing antibiotic stewardship and educating patients about the importance of using antibiotics safely and appropriately.
The survey report can be accessed here.